The road towards UHC in Kurdistan region of Iraq: Challenges and hopes for the future
2023-03-29
Dr. Goran Zangana MBChB, MPH, PhD
Mr. Bestoon Fatah
Mr. Azaden M. Amin
INTRODUCTION
To celebrate the Universal Health Coverage (UHC) day in Iraq, a meeting was convened in Slemany on 12/12/2022. The meeting was organized by the HUMAN Network for Health and Humanitarian Affairs (HUMAN) in partnership with the Sustainable Development Network (SDN) of the Kurdistan region of Iraq. Many stakeholders including representatives from the Ministry of Health (MoH), Local Municipality Council,
WHO-Iraq, members of parliament and representatives of civil society organizations in the country (for full list of attendees please refer to Annex 1).
The objectives of the meeting were as follows:
Celebrate UHC day in Iraq
Raising awareness about UHC among multiple government, non-government and private sector actors in the country
Reviewing the progress of the country towards UHC2030
Initiating efforts to formulate an action plan for supporting efforts towards UHC in Iraq.
Background:
There is a dearth of knowledge and data exploring indicators related to UHC in Iraq. However, there is still some information on the topic that can be useful for policymakers, academia, civil society and other actors.
Figure 1, shows the worsening indicators in terms of catastrophic health expenditure in
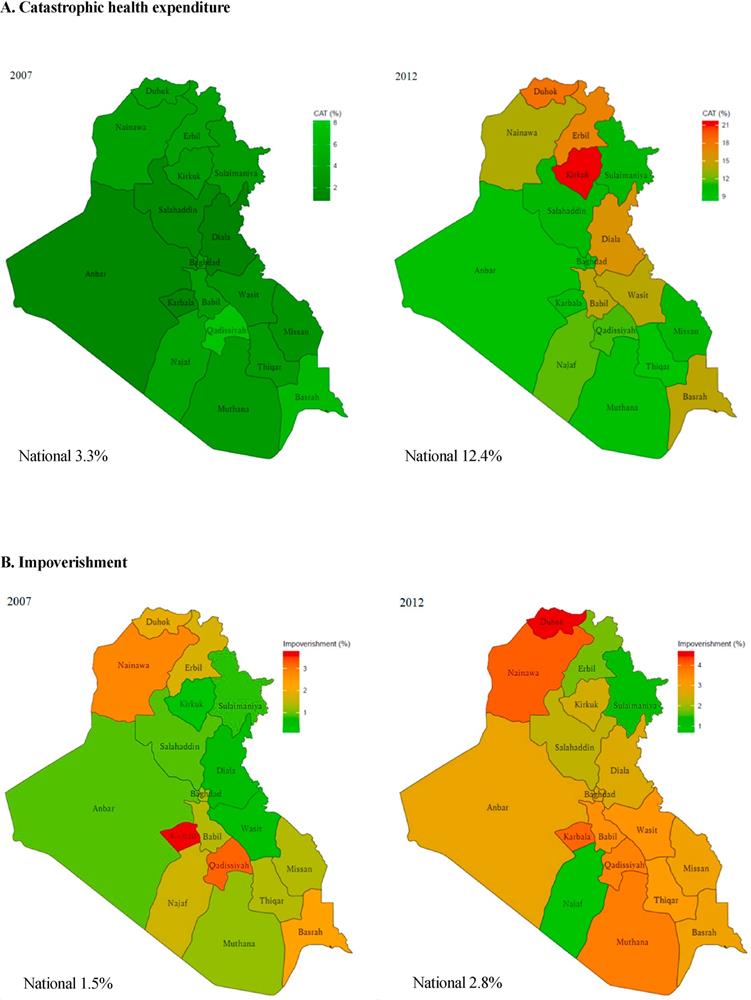
Iraq. source
Figure 1: financial risk protection indicators in Iraq, 2007 and 2012. CAT, catastrophic health expenditure.
Source: https://www.sciencedirect.com/science/article/pii/S0277953620308492
Figure 1 shows the incidence of catastrophic health expenditure has increased in Iraq between 2007 and 2012. The figure shows that in parallel with that increase in catastrophic health expenditure there has also been an increase in improvement.
At least in part, these worse indicators are correlated with the increasing out-of-pocket expenditure on health.
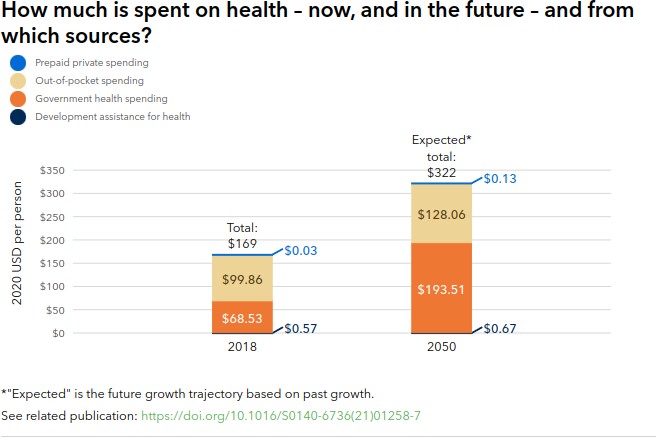
Figure 2: Healthcare expenditure in Iraq in 218 and projection for the future source : https://www.healthdata.org/iraq
Figure 2 shows that government health spending constituted a little more than one third of the total spending on health in Iraq. The other two third is coming from out-of-pocket expenditure.
This poor government investment is unsurprisingly translated into poor service coverage (Figure ).
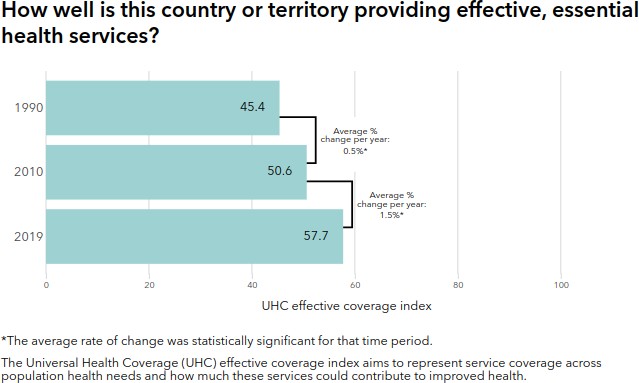
Figure 3: providing essential health service source: https://www.healthdata.org/iraq
Figure 3 shows that less than 60% of the population in Iraq is covered by effective coverage. Although there has been an improvement in coverage, it is both slow and leaves a substantial proportion of the population.
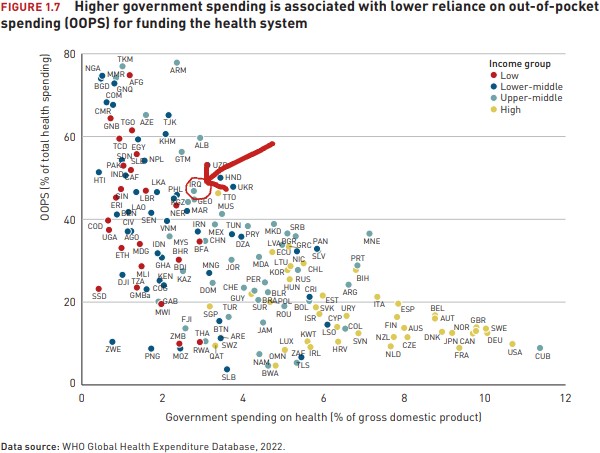
Also, on the international level, Iraq is not doing very well in comparison with other countries (Figure 4).
Meeting proceedings
The meeting included speeches, focus group discussions and lessons learned and plans for the future (for the agenda of the meeting, please refer to Annex 2)
The following speeches were delivered: (for photos of speakers, participants and presentations please refer to Annex 3)
Mr. Bestoon Fatah, Head of the health unit at SDN
Dr Herish Salim, Deputy Director of the Directorate of Health of Slemany Governorate
Mr. Hussam Barzanji, Coordinator of SDN
Mr. Izzadin Muhamad Amin, Director General of HUMAN Three focus groups were convened:
Climate change determinants of health
Public health group
Community and civil society engagement group
The event was covered in national and local media (for links to media coverage of the event please refer to Annex 4)
Topics of discussion:
The changing epidemiological landscape:
The participants highlighted the changing epidemiological demographics of the country. One example that was highlighted was the increasing numbers of patients with a cancer diagnosis (Figure 5)
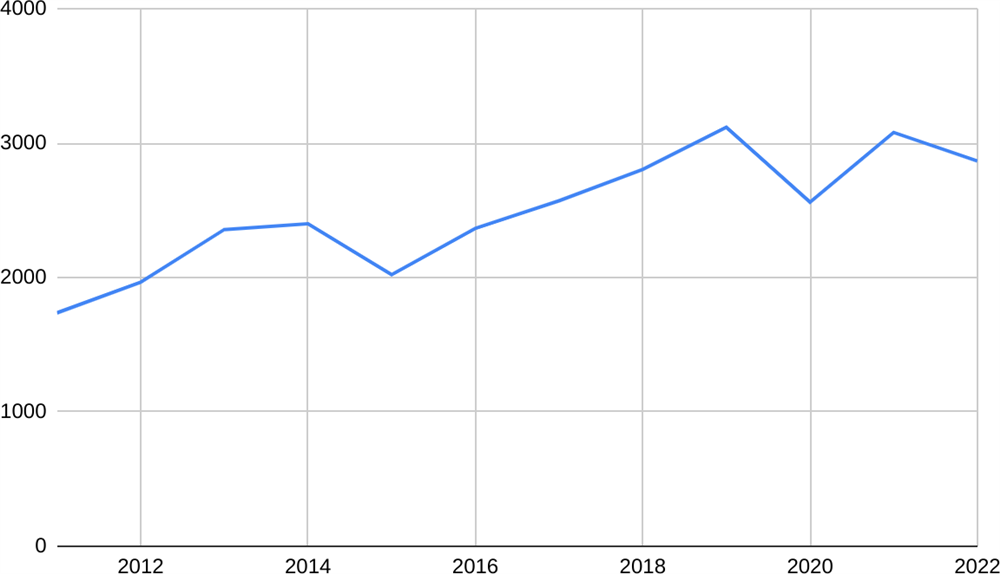 Figure 5: shows the increased number of cancer diagnosis in the governorate of Slemany
Figure 5: shows the increased number of cancer diagnosis in the governorate of Slemany
The increased numbers of cancer diagnosis were highlighted as a factor in increasing the out-of-pocket expenditure for paying often expensive healthcare services for this diagnosis. However, there is no available data which specifically measures the catastrophic health expenditure related to cancer diagnosis in the country.
Health financing:
The participants discussed the fact that the Government of Iraq (and its Kurdistan regional government) only spend 3-5% of the Government budget on healthcare. This has resulted in an increase in regressive sources of financing such as out-of-pocket expenditure.
Another way that the population and other organizations have to resort to in the absence of adequate government investment has been what is known as the ‘Cancer fund’ for oncology treatment. Philanthropists, businesspeople, patients and families have been contributing to this fund to cover the cost of treatment for cancer patients. However, it has been reported that those funds are being abused for private gains. Participants called for investigations into those alleged abuses.
In addition to these voluntary arrangement for resource generation, the government has also imposed what has become known as the ‘semi-private’ scheme. According to this, public facilities offer discounted services only for few hours in the mornings. After 12 pm, services become charged at the private market prices. This scheme was introduced in 2014 as a reaction to low oil prices, security crisis of ISIS and a resulting economic crisis in the country. However, this scheme has been criticized by many participants as a source of corruption, waste and injustice. Participants called for abolishing this scheme given that it is unconstitutional (Iraqi constitution guarantees access to healthcare) and improving economic conditions.
The health system and policy landscape
Participants stressed the increased size and role of the private sector in the country. They recognised that as a source of catastrophic expenditure in Iraq. Furthermore, participants also highlighted the role of such an increased role of the private sector on health policy. For example, some participants underlined conflict of interest in relation to promoting business interests in the public sector.
Some participants highlighted issues with social participation, people-centeredness and community engagement in the health system. One participant argued that the Ministry of Health is the Ministry of Doctors rather than the public. She provided the lack of accountability for medical errors (which is costing money, lives and health) as evidence for the dominance of the doctors in health policy.
One participant unscored the politicization of the health system through monopoly of senior positions and contracts to political parties and persons. This was seen as a source
of corruption and waste in the system through the appointment of less qualified persons. Also, awarding contracts to political connected companies was highlighted as another source of waste and corruption in the system. Furthermore, this factor was identified as a cause for the importation (and sometimes smuggling) of counterfeit, substandard or expired medicines and food items by politically connected individuals and companies which in turn is causing adverse health effects and wastage in terms of failure to tax those smuggled commodities.
Recommendations:
Financing:
Increasing the investment of the government in public health to at least 10% of the Iraq national budget. Alternative methods of resource generation through taxation of harmful substances should be considered.
Pooling of financial resources through social health insurance.
Designing healthcare expenditure policies that align with the functions of equity, primary health, performance and quality.
Governance:
The cessation of the politicization of the healthcare system.
Introduction of long term strategic plans for health reforms in the country
The creation of circumstances to move away from the biomedical model of health governance
Democratization of health governance through encouraging and facilitating community and social participation in decision making.
Combating corruption, waste and nepotism in the healthcare system
Healthcare workforce:
Introducing job descriptions and pay for performance schemes
More equitable distribution of the healthcare workforce
Improving the living conditions of healthcare workforce through increasing salaries and incentives